159 Ravali Irugurala
General medicine
21/0ct/ 2021
Name : Ravali Irugurala
Roll no : 159
3rd sem student
This is an online e log book to discuss our patient de- identified health data shared after taking his/ her guardians signed and informed consent.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Case presentation:
A 74 yr old male , retired RTC driver(11 yrs back) , resident of narketpally came to the casuality with complaints of fever since 3 days , decreased urine output since 2 days,SOB GRADE :3 since 1 day.
History of present illness:
1.FEVER:
- Sudden in onset, associated with chills, increased during nights & relieved on medications.fever spikes increased after connecting urine bag before 2 days
2.DECREASED URINE OUTPUT:
- Normal frequency was 4 times/day & 3 times/night.since 2 days from tuesday morning, output decreased.they went to local RMP at night 10pm of tuesday & urine bag was connected by local RMP.
3.SOB GRADE : 3
- Present while walking & at rest also
Past History:
Pt was apparently asymptomatic 2 months back, was admitted & diagnosed in our hospital with Lft facial nerve palsy, peripheral neuropathy(? ATT INDUCED), denovo HTN (? post pulmo tb), Spondyloarthropathy with radiculopathy sacroileitis cervical OPLL ( Ossification of posterior longitudinal ligament) - Ankylosing spondylitis
- k/c/o DM - 2 Since 20 yrs.
Personal History:
DIET: vegetarian
APPETITE : decreased since 1 month
SLEEP: decreased since 2 days
BOWEL & BLADDER MOVEMENTS : urine decreased
ADDICTIONS : smoking present since 20 yrs ( 3 packets/day ) stopped 5 yrs back
VITALS:
Temperature: febril
PR: 98 bpm
RR:22 Cp
BP : not recordable
Spo2: 98%
General examination:
No pallor, icterus, cyanosis, clubbing, lymphadenopathy,pedal edema
Systemic examination:
CNS: FNAD
CVS: S1 &S2 heard ,no murmurs
Respiratory system: NVBS
PERABDOMEN:
Soft , tenderness & pain present
Abdominal distension: present
Investigations:
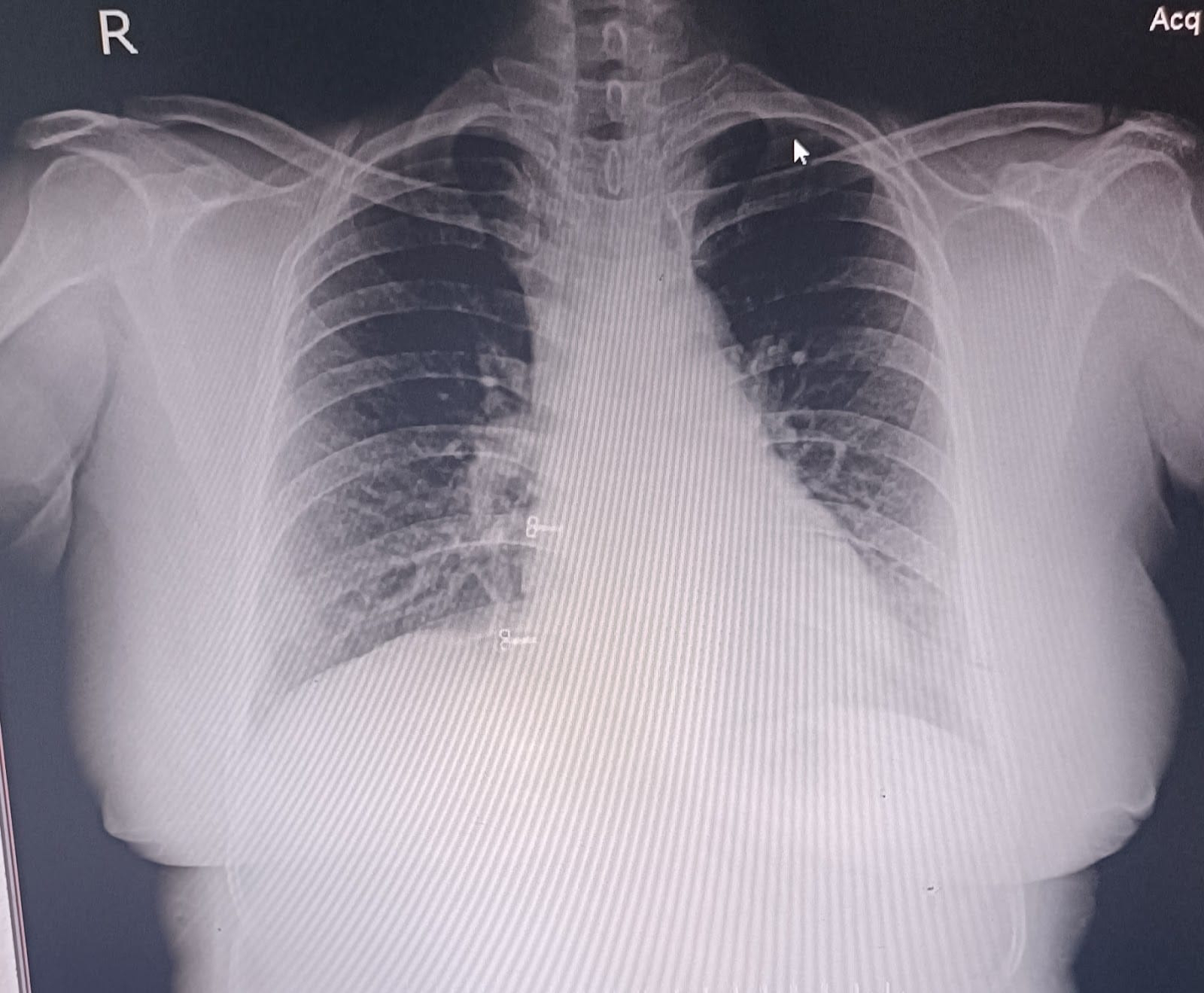
Chest x ray:
2 D echo report:
ABG report:
Liver function test:
Serum electrolytes:
Blood urea:
Serum creatinine:
PROVISIONAL DIAGNOSIS:
AkI (pre renal / renal ) on CKD k/c/o HTN /DM cervical myelopathy.altered sensorium secondary to metabolic (? Hepatic/ uremia)
TREATMENT:
On 21/010/21
•INJ.PIPTAZ 2.25/ IV / TID
•INJ.PAN 50 mg /IV/OD
•INJ.ZOFER 4mg /IV/SOS
•INJ.PCM.1gm /IV/SOS
•INJ.NOR-ADREANALINE 10ml/hr NS
Patient suddenly became unresponsive at today 7:00 pm with no cardiac activity
CPR was initiated acc to 2015 AHA guidelines and intubated with ET 7.0 ROSC obtained after 5 cycles of CPR and patient was put on mechanical ventilator
ACMV-VC
Fio2: 100
RR: 14 cpm
VT: 420ml
PEEP: 5cms
Post intubation vitals:
PR: 110 bpm
BP: 70/40 mmhg
Spo2: 98%
CVS: s1 s2 +
RS: BAE + , NVBS
P/A: Soft , BS +
ECG report after 1 hr:
At 1:35 AM on 22/10/21 patient again became unresponsive with no cardiac activity
CPR initiated acc to 2015 AHA guidelines and continued for 6 cycles.
Inspite of all the resuscitative measures patient could not be revived and declared dead at 2:05 AM on 22/10/21










Comments
Post a Comment