159 Ravali Irugurala
General medicine
11/11/22
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's consent.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box below.
Note : This is an ongoing case and will be updated regularly.
Date of admission: 9/11/22
Case presentation:
A 14 yr old boy came to the opd with complaints of pain abdomen in the left side of the abdomen since the past 15-20 days
Chief complaints:
He was having pain abdomen and noticed a swelling in the left side of the abdomen since the past 15-20 days.
HOPI:
Patient was asymptomatic till 9 years of age. At 9 years of age August, 2016 - parents noticed neck swelling and he had difficulty in swallowing they took him to ENT doctor ,later referred to endocrinologist ,where he was diagnosed with hyperthyroidism.
USG showed diffuse enlargement of both lobes of thyroid gland with altered echotexture ?Goitre with bilateral jugular lymphadenopathy. FNAC was done showing features suggestive of hyper plastic goitre.
Initial TSH - 0.57, T3,T4 was 217 and 1.8 respectively.
he was started with propylthiouracil 50 mg and was asked to review back as of October 2016,
TSH was >150 and T3 - 12, T4 was <0.3 and was started intitially on thyroxine supplementation of 25mcg later on increasing to 150,180 and 200mcg over 6 months.
At 12 years of age patient had chicken pox, resolved over 10 days.
Around late part of December 2021
He gave history of yellowish discoloration of eyes, One episode of bilious vomiting. yellow coloured urine, He was treated by a pediatrician (family doctor) for jaundice ,but as the bilirubin was on increasing trend he was referred to our hospital in the first week of January with the history of above said complaints of 7-10 days.
Past history :
N/k/c/o diabetes, CVD, epilepsy , asthma
K/c/o thyroid disorder
Personal history:
Sleep : adequate
Appetite: normal
Bowel & bladder : H/o 4 episodes of loose stools on 10/11/22.
No known allergies
No addictions
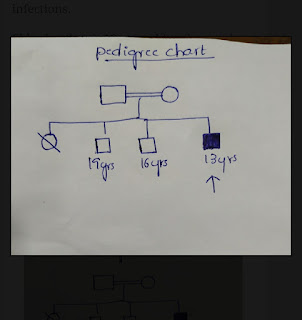
Family history:
He is a 4th order child ,born out of grade 4 consanguinous marriage, He has 2 elder brothers and one elder sister - who expired at 5 years of age, His sister was the first child and she was assymoptomatic till 2 years of age ,then she had shortness of breath and was rushed to hospital,where here condition detiorated and got admitted .They were told that she had splenomegaly and Her blood counts were decreasing .She was given multiple blood transfusions every 25 days for one year inspite of that she remained anemic ,she also underwent bone marrow biopsy twice . According to parents she was given steriods also for one year before death .she never had jaundice or recurrent infections.
Elder brother is 19 year old and second brother is -16 years old . Second one had history of fever ,white coloured loose stools at the age of 5 years ,for which they went to near by hospital .He was given some medications and it got resolved .But he was said to have anemia ,and he recovered according to parents with some medications.There was no jaundice and no history of blood transfusion.
GENERAL EXAMINATION
On Examination, the patient is conscious, coherent and cooperative
▪︎Moderate built and nourishment
▪︎No signs of pallor, icterus ,cyanosis, clubbing, koilonychia, lymphadenopathy, edema of feet
VITAL SIGNS
•Temperature :97.4°F
•BP :110/70 mmHg
•Pulse:82 beats per min
•Respiratory rate:16 cycles per min
SYSTEMIC EXAMINATION
CVS:
Cardiac sounds S1,S2 heard
No Cardiac murmurs
RESPIRATORY SYSTEM :
No dyspnoea, wheezing
Position of trachea-central
NVBS present
PER ABDOMEN :
INSPECTION
Shape of abdomen- scaphoid
Umbilicus normal
•No engorged veins, visible peristalsis,scars and sinuses
PALPATION
. All inspectory findings are normal
. No tenderness seen
. Palpable mass felt- massive splenomegaly
CNS:
Speech- normal
No signs of meningial irritation
Investigations:
Serum creatinine
Liver function test
Serum electrolytes
Complete urine examination
APPT








Comments
Post a Comment