159 RAVALI IRUGURALA
4-dec-2023
60 YEAR OLD MALE CKD ON MAINTENANCE HEMODIALYSIS WITH ANEMIA OF CHRONIC KIDNEY DISEASE WITH HYPERTENSION
A 60 year old male, who is a resident of Nalgonda ,farmer by occupation came with
Chief complaints :
Pedal edema since 3 months.
Shortness of breath since 20 days. Decreased urine output since 15 days.
History of presenting illness:
The patient was apparently asymptomatic 3 months back when he noticed bilateral pedal edema initially extending to ankle Gradually progressed up to thighs which worsened during last 15 days.
Decreased urine output since 15 days, not associated with frequency, urgency burning micturation.
Grade 3 shortness of breath, no aggravating and relieving factors.
Before the presenting illness :
Patient had History of trauma by fall from tree 17 years back, where he used NSAIDS for 4/5 yrs ..
Then 12 years back he developed pedal edema where He got diagnosed that he had kidney problem and he was on medication and where edema was subsided and it was more recurrent on those 5 years.
Then he was diagnosed with CKD For which he got treated by dailysis initially and then he started using medications
Patient was apparently well till 3 months back
3 months back patient developed bilateral pedal edema, facial puffiness for the first time and shortness of breath so he visited local hospital and they referred to our hospital for dailysis.
Since then patient was coming here regularly twice a weak for dialysis .
After his last dialysis session he went back home and he developed discomfort in chest and weakness of limbs . Patient also had few episodes of altered sensorium in between.
So he was brought to hospital again.
PAST HISTORY:
Known case of hypertension since 6 months
No history of diabetes mellitus, asthma, cardiovascular disease , epilepsy, tuberculosis
There is a history of blood transfusions.
PERSONAL HISTORY:
Mixed diet
Sleep adequate
Bowel-Regular
Bladder-Irregular
No known allergies
consumes alcohol occasionally
Smokes tobacco
DAILY ROUTINE
Before 3 years :
Wakes up at 5 am and goes to field and toddy trees
Breakfast at 9 am -rice
Afternoon- lunch 12 pm
Evening drinks toddy
And dinner by 9 pm and sleep
Now :
Wake up at 8 am
Breakfast at 9 am
Skips lunch and dinner at 8 pm
He is not going to work,not as active as in the past
FAMILY HISTORY:
Father had Hypertension.
No history Tuberculosis, diabetes mellitus,etc.
GENERAL EXAMINATION:
Patient is conscious, non coherent,
non cooperative.
Gynaecomastia present.
pallor present.
clubbing is seen
No signs of icterus , generalized lymphadenopathy.
signs of bilateral pedal edema.( Pitting)
Pallor
Pedal edema
Clubbing
VITALS
Temp:100 F
PR: 98
RR: 29/ min
Bp:100/80 mm Hg.
Spo2: 84%
GRBS:124 mg/dl
SYSTEMIC EXAMINATION:
Cardiovascular system:
S1,S2 heard , no mumurs.
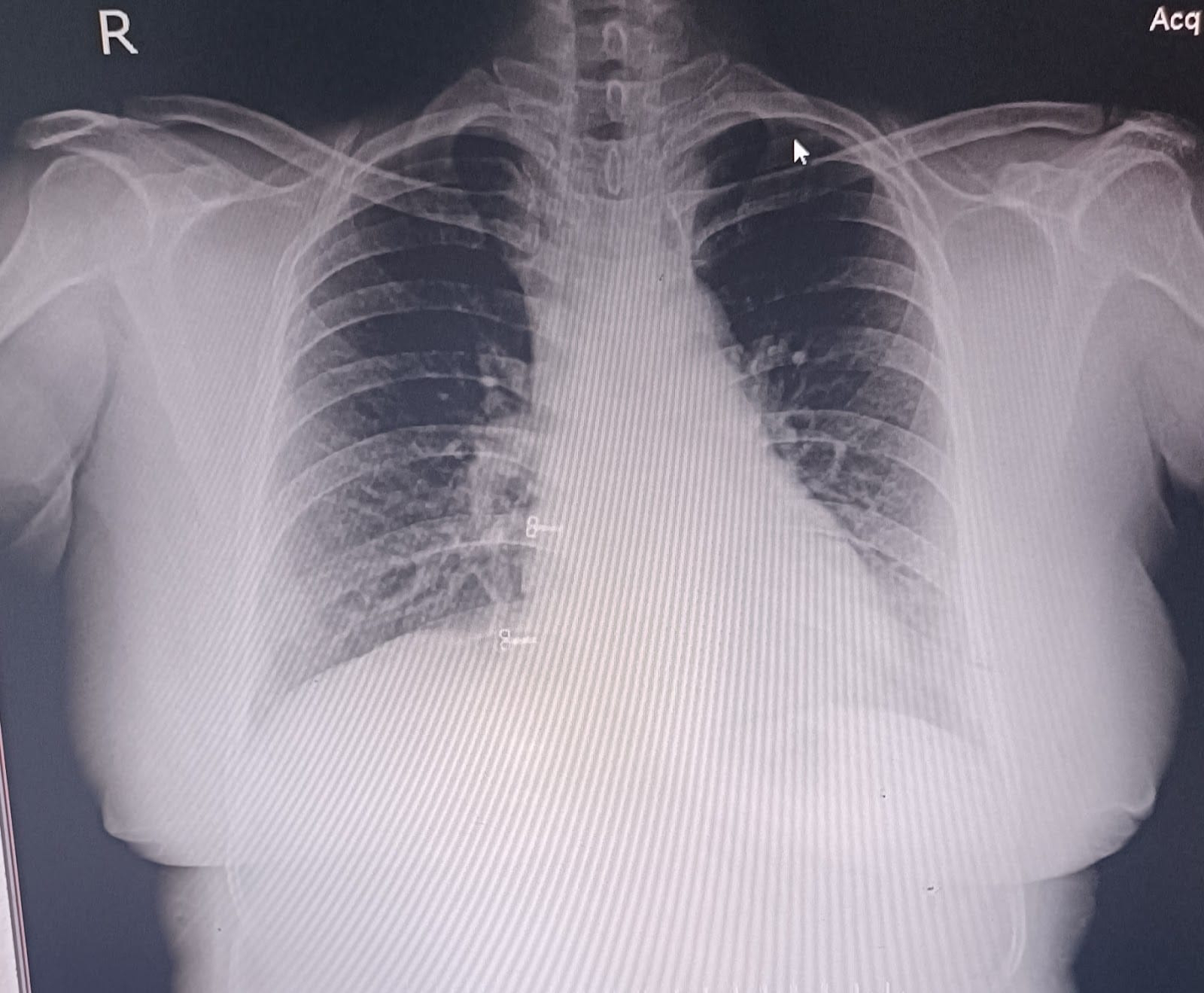
Respiratory system:
Position of trachea central.
Bilateral airway entry present.
Dyspnea present
No wheeze.
Abdomen:
Scapoid
No tenderness
No palpable mass
CNS examination:
Patient has altered sensorium and he seems to be irritable, non cooperative
Slurred speech
No delusions , hallucinations
MOTOR SYSTEM EXAMINATION
Bulk
Rt Lt
Upper limb
MAC 26 cm 26 cm
MFAC 23 cm 23 cm
Lower limb
MTC 33 cm 33 cm
MLC 28 cm 28 cm
Tone
Upper limb
Hypertonia in both right and left (3/5) Lower limb
Hypertonia in both right and left (3/5)
Power
Upper limbs - in right and left grade 3
Lower limbs - in right and left grade 2
Reflexes
Biceps - Normal in both right and left
Triceps - Normal in both right and left
Supinator - Normal in both right and left
Knee jerk relfex - Not elicited
Ankel reflex - Not elicited
Plantor relfex - Not elicited
CEREBELLAR SIGNS :
Finger nose test -abnormal
Dysdiadochokinesia-
Heel knee test -abnormal
PROVISIONAL DIAGNOSIS:
chronic kidney disease on maintenance hemodialysis with anemia secondary to chronic kidney disease with hypertension. uremic encephalopathy ? under evaluation
INVESTIGATIONS
On 28/11/2023
Hemogram
RFT
Serology
ECG
On 29/11/2023
Hemogram
RFT
ABG
Hemogram
Hemogram
TREATMENT
Patient was on salt restriction < 1.5 g / day
Patient was on fluid restriction <1.5l per day
Inj : PIPTAZ 2.25 gm iv /tid
Inj LASIX 40 mg iv /bid
Inj MEOMOL 14 mg iv sos if temp >101
Tab : ECOSPRIN 50mg H/S
Tab : OROFER once a day
Tab DOLO 650 mg every 6 hourly
Tab NODOSIS 500 mg PO /BD
Tab SHELCALT 500 mg /BD
On 29/11/23
TAB. LINOD 10mg twice a day.
Inj LASIX : 40 mg Iv twice a day
Tab : Oral NODOSIS 500 mg twice a day
Tab: Oral SHELCAL 500 mg twice a day
Inj.EPO 4000 IU ,SC once weekly
Tab : oral ECOSPRIN 75mg H/S
Inj NEOMAL : 14mg IV sos
Tab : DOLO 650 mg QID
Inj PIPTAZ : 2.25 gm I.v thirice a day
On 30 /11/23
Treatment
Inj PIPTAZ : 2.25 gm I.v twice a day.
Inj LASIX : 40 mg Iv twice a day
Inj NEOMAL : 14mg IV sos
Tab : Oral NODOSIS 500 mg twice a day
Tab: Oral SHELCAL 50 mg twice a day
Tab : oral ECOSPRIN 50mg H/S
Tab OROFER once a day
Tab : DOLO 650 mg QID
Intermittent CPAP
Oxygen supplementation 1-2lts





















Comments
Post a Comment